Flush away chronic constipation with magnesium oxide, kiwifruits and psyllium
Key takeaways
- The guidelines recommend kiwifruit, rye bread, psyllium fiber, magnesium oxide, and certain probiotics for managing chronic constipation.
- Researchers find limited evidence supporting generic high-fiber advice and supplements for constipation relief.
- The evidence-based framework aims to help patients and clinicians adopt more effective, personalized dietary management strategies.

Researchers at King’s College London, UK, have published the “first-ever” evidence-based dietary guidelines for adults with chronic constipation. It includes kiwifruits, rye bread, high-mineral-content water, and supplements like psyllium fiber, magnesium oxide, and certain probiotic strains.
The more common and widely recommended approaches to this bowel issue are too generic — eat high-fiber diets — or lack strong evidence of effectiveness for senna supplements, a type of laxative, note the researchers.
Additionally, they critique common clinical guidelines for being limited and sometimes outdated with dietary recommendations, which typically focus on increasing dietary fiber and fluid intake.
The guidelines published in the Journal of Human Nutrition & Dietetics and Neurogastroenterology & Motility seek to change the way doctors, nurses, and dietitians manage chronic constipation in clinical practice to enable better symptom self-management through diets.
“For dietary supplements, 15 recommendation statements relate to fibre supplements, 20 relate to probiotics, 2 to synbiotics, 5 to magnesium oxide, 2 to senna, and 3 to kiwifruit supplements,” reads the paper.
Senior author Kevin Whelan, professor of dietetics says: “This new guidance marks a promising step toward empowering health professionals and their patients to manage constipation through diet.”
“This means that from now on, people suffering from constipation across the world can now receive up-to-date advice based upon the best available evidence in order to improve their symptoms and well-being. With continued research, it holds real potential to drive lasting improvements in quality of life.”
Quality of life
Chronic constipation is a common, long-term condition that significantly lowers quality of life, the researchers add. Patients and healthcare are also found to face high financial burdens.
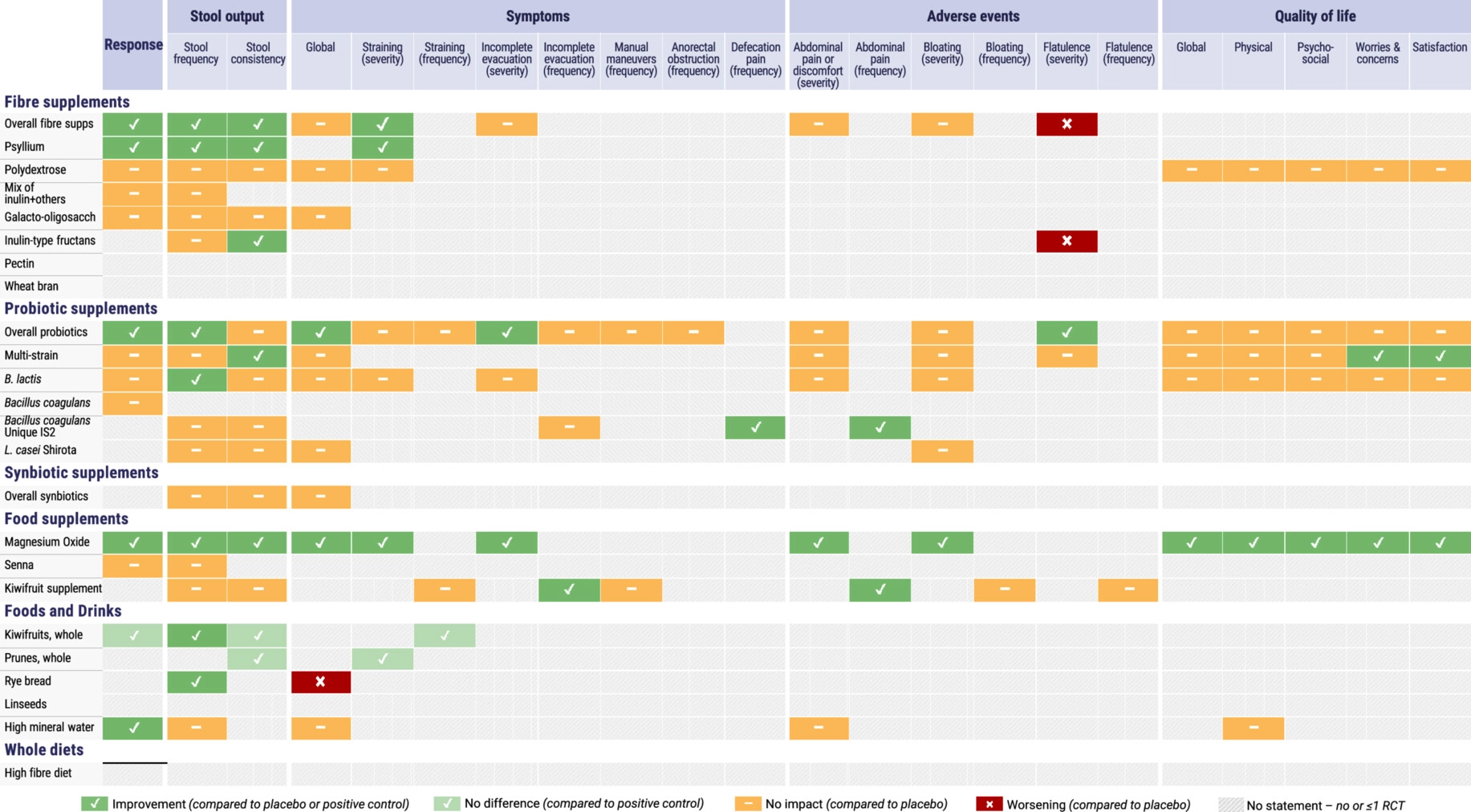 A clinician-friendly summary guide of the recommendation statements as a practical tool that facilitates the adoption of the guidelines in clinical practice (Image credit: Journal of Human Nutrition & Dietetics).“Chronic constipation can have a huge impact on someone’s day-to-day life. For the first time, we’ve provided direction on what dietary approaches could genuinely help and which diet advice lacks evidence,” comments lead author Dr. Eirini Dimidi, Reader in Nutritional Sciences.
A clinician-friendly summary guide of the recommendation statements as a practical tool that facilitates the adoption of the guidelines in clinical practice (Image credit: Journal of Human Nutrition & Dietetics).“Chronic constipation can have a huge impact on someone’s day-to-day life. For the first time, we’ve provided direction on what dietary approaches could genuinely help and which diet advice lacks evidence,” comments lead author Dr. Eirini Dimidi, Reader in Nutritional Sciences.
“Being able to improve this condition through dietary changes would allow people to self-manage their symptoms more and, hopefully, improve their quality of life.”
Evidence-rooted guidelines
The researchers tout that the new guidelines are rooted in systematic reviews and meta-analyses and apply the GRADE framework to assess the quality of the evidence — unlike previous guidelines.
The recommendations also share outcomes like stool frequency, consistency, and straining. According to the researchers, this makes them more personalized and practical based on each person’s specific symptoms. The guidelines are supported by a clinician-friendly tool.
According to the review, some foods and supplements are effective in treating chronic constipation; however, the overall quality of studies is low. Most trials were found to focus narrowly on single interventions instead of diet approaches. The researchers call for better nutrition research in this space.
“Eating a high-fiber diet offers many benefits to overall health and has been a go-to recommendation for constipation. However, our guidelines found that there simply isn’t enough evidence to suggest it actually works in constipation specifically,” says Dimidi.
“Instead, our research reveals some new dietary strategies that could indeed help patients. At the same time, we urgently need more high-quality trials to strengthen the evidence on what works and what doesn’t.”

















